The Complicated Legacy of Terry Wallis and His Brain Injury
An Arkansas man’s unprecedented recovery of consciousness, and his recent death, demonstrate why progress in neuroscience must be matched by new standards of care for patients as well as attention to their civil rights.
In the eight years that I have been teaching a seminar on disability rights and brain injury at Yale Law School, I have never come close to tears. But last April I choked up when I told my students about the death of Terry Wallis, at age 57, on March 29, 2022. Wallis, who came to international attention when he awakened from what was thought to be a permanent vegetative state after 19 years of being unresponsive, was well-known by my students—his astonishing experience anchors what I hope will become legal frameworks that enable disability law to better meet the needs of patients with severe brain injury.
After an accident in 1984, Terry was considered by his care team to be in a state of permanent unconsciousness, until 2003—when he said “Mom” and then “Pepsi,” his favorite drink. It’s not an exaggeration to say that Terry’s awakening set off a “golden age” of brain science, profoundly changing the scientific, moral, ethical, and legal understandings of consciousness. Although Terry was exceptional—he became a brain injury rock star—his death was all too ordinary and, arguably, avoidable: a consequence of therapeutic nihilism about severe brain injury, widespread discrimination against people with disabilities, and inadequate rehabilitation facilities in the rural area where he lived.
The irony and injustice of the way he died affected me deeply. Despite the fact that neuroscience has learned so much from Terry’s remarkable journey, the United States’ depersonalized health care system neglected him, like so many others with severe brain injury. His death was a harsh reminder that the revolution in brain science that Terry helped launch will remain incomplete until scientific progress is matched by an obligation to bring these advances into clinical practice in ways that are meaningful and just.
In the months since his passing, I have come to think that Terry’s death in 2022 may be as important as his emergence in 2003 for the way it encapsulates both the progress and peril of how society is coming to understand severe brain injury and frame its obligations to care for people who have experienced them.
Lauching a Golden Age
I first met Terry and his parents, Angilee and Jerry, when they came to the Consortium for the Advanced Study of Brain Injury at Weill Cornell Medicine and Rockefeller University in 2004 to see if our team, which I codirect with neurologist Nicholas D. Schiff, could explain his emergence. I interviewed Angilee and Jerry as part of research for my book on the rights of those with severe brain injury, Rights Come to Mind, shortly after they arrived in New York from rural Arkansas. I gathered they felt out of place in Manhattan, but we immediately struck a connection when they realized that their concern for Terry was matched by our research group’s interest in his experience.
“The revolution in brain science that Terry helped launch will remain incomplete until scientific progress is matched by an obligation to bring these advances into clinical practice in ways that are meaningful and just.”
The Wallis family was familio-centric: nothing was more important than Terry, whose medical course Angilee had tracked carefully since his car accident. She told me that the family thought they had seen glimmers of awareness over the years and had asked for a neurologist to reassess Terry’s condition, only to be told it was too expensive and wouldn’t matter.
Terry’s remarkable story had garnered international headlines and been hailed as a miracle, but my colleagues and I were not surprised by his recovery. Although he had been described as being in the vegetative state—that is, permanently unconscious—we suspected he had actually been in the minimally conscious state (MCS), a condition that was only formalized a year before Terry started to talk again.
MCS resembles the vegetative state but is distinct because MCS patients are conscious, albeit liminally so. They have awareness of self, others, and the environment. The challenge is that they don’t always manifest these behaviors and can appear vegetative when these signs are absent. But biologically, these patients are distinct from those in the vegetative state. The minimally conscious brain is functionally integrated and capable of communicating across widely distributed neural networks necessary to sustain consciousness. This contrasts with the functionally disintegrated vegetative state, which cannot work as a consolidated unit and thus cannot sustain consciousness. In contrast, MCS patients exhibit behaviors reflective of awareness and consciousness: they may say a word, reach for a cup, or look up when you enter the room. However, these behaviors are usually episodic and intermittent, and such signs of covert consciousness are easy to miss. One study found that up to 43% of nursing home patients diagnosed as vegetative following traumatic brain injury were in fact in MCS.
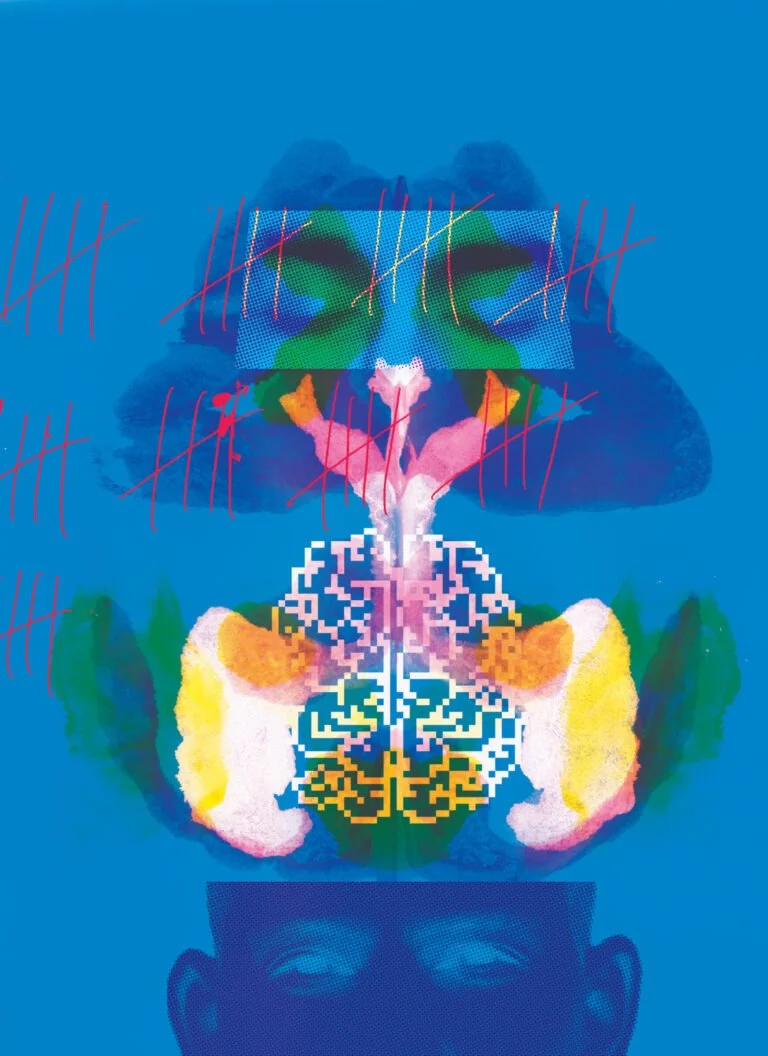
Before we even met Terry, we guessed that he had been in MCS, which meant that during the many years that he was lying in his nursing home bed, his brain had recovered. Imaging studies of Terry’s brain done by Schiff and our team found dynamic changes that might explain the improvement in his brain state. These included possible axonal regrowth of the white matter fibers that connect nerve cells—a phenomenon normally seen in children’s brains as they develop. This suggested that his neurobiology was adaptive: a developmental process was being reharnessed in service of repair and regeneration. This hypothesis was later confirmed in a longitudinal study published in 2016 that tracked another patient as she regained an ability to communicate over the course of 54 months.
Terry’s scans were stunning, revealing the potential of the injured brain to heal itself and carrying implications for how physicians view the depth and length of rehabilitation. If brain recovery recapitulates brain development, which takes years, maybe the duration of rehabilitation should resemble that of childhood education, which is tailored to the developing brain. If rehabilitation is viewed as analogous to the educational process, then payments for its provision should be guided by the underlying recovery. Instead, they are often guided by the traditional reimbursement criteria of insurance companies, which presume stasis—often resulting in patients having to forgo rehabilitation efforts altogether. Brains recover by biological mechanisms, not reimbursement criteria.
“Terry’s scans were stunning, revealing the potential of the injured brain to heal itself and carrying implications for how physicians view the depth and length of rehabilitation.”
In the two decades since Terry regained his voice, the science of disorders of consciousness—and the possibility of treatment—has radically shifted. Researchers have learned how to identify covert consciousness with functional neuroimaging, begun to develop drugs and devices that can accelerate the return of consciousness, and now even consider the ethical implications of these advances. This progress culminated in 2018, when a new standard of care for patients with disorders of consciousness was issued by the American Academy of Neurology, the American Congress of Rehabilitation Medicine, and the National Institute on Disability, Independent Living, and Rehabilitation Research. In addition to the use of emerging technology and drugs to assess and treat patients, the new standard importantly called for the amelioration and prevention of confounding conditions that effect the morbidity and mortality of these patients, such as bedsores, urinary tract infections, and pneumonia. If a patient succumbed to these conditions because of inadequate care, any progress in the diagnosis and treatment of their underlying brain injury would be for naught.
It was clear that Terry’s awakening had helped catalyze a promising era of neuroscience and prompted a moral consideration of what society’s responsibilities should be toward people with severe brain injury. Indeed, as the personification of MCS and example of what neuroscience was learning about severe brain injury, Terry’s passing was a major news event: the New York Times carried a full obituary with a photo, and I saw him featured as a “notable death” on a national TV news show.
An Unworthy Death
These cultural markers, however, only tell part of Terry’s story—celebrating his emergence. They don’t acknowledge how he died. And Terry’s notoriety makes the circumstances of his death all the more disquieting. With access to adequate care, I believe the complications that led to his death might have been prevented and treated. But for patients with brain injuries, who are often subject to what is euphemistically called “custodial care,” such deaths are all too common. These gaps in care are the bleak companion to an emerging golden age of brain science. A systematic review published in 2018 revealed that the number of patients with prolonged disorders of consciousness admitted to inpatient rehabilitation had “progressively declined” over the previous 15 years. Access to high-quality rehabilitation is limited by geographic availability and insurance preauthorization requirements that tend to send such patients to nursing facilities rather than rehab. Thus there is a paradox: scientific progress over the past two decades has not been matched by correlative access to the latest standards of care. Without adequate rehabilitation, patients cannot benefit from advances in neuroscience.
“In the two decades since Terry regained his voice, the science of disorders of consciousness—and the possibility of treatment—has radically shifted.”
In January 2022, Terry developed pneumonia. Before participating in a decision to place him on a ventilator, his sister, Tammy Baze, called Schiff and me for advice. Tammy said that his doctors advised against the procedure because they couldn’t imagine that the life he led was worth living. But Terry had treatable pneumonia, and his family insisted he be treated like anyone else.
Later the family told us that doctors asked to remove the ventilator, saying that Terry seemed withdrawn—which they ascribed to the hopelessness of his brain injury. However, his family felt that his interactions with them hadn’t changed, but rather that he was still grieving his mother Angilee, who had died two years earlier. Furthermore, he couldn’t fully articulate his feelings with a tracheostomy in his airway. The family felt that because they couldn’t clearly understand his wishes, it would be wrong to withdraw life support.
Based on what the family told us, Schiff and I said that Terry needed access to pulmonary rehabilitation to regain lung function. A new doctor agreed, but there were no facilities nearby that had availability and were capable of providing the kind of rehabilitation he needed. There seemed to be a place out of state, but Terry was too frail for a long ambulance ride. He was transferred to a skilled nursing facility that could provide pulmonary support until he was strong enough to make the trip. Despite the best efforts of his family and care team, he died of pulmonary complications.
“Scientific progress over the past two decades has not been matched by correlative access to the latest standards of care. Without adequate rehabilitation, patients cannot benefit from advances in neuroscience.”
It would be a shame if the public only remembered Terry’s awakening and failed to acknowledge the policy implications of his death. Even though Tammy advocated for Terry and rallied support from his care team, without access to rehabilitation locally, his treatment was predicated on him becoming well enough to travel out of state. All of this speaks to the intersectionality—and compounding vulnerability—felt by people with severe disabilities. These challenges are amplified by poverty, limited access to health care in rural America, and historic crosscurrents about vulnerable people’s right to die and right to care. Safeguarding the rights of people with disabilities is especially critical when their lives are marginalized by so many complicating factors.
I didn’t get the chance to go to Terry’s funeral, which was near his home in Big Flat, Arkansas. He was buried next to his mother and—reflecting his sense of humor and his favorite soft drink—he wore a Pepsi shirt and his casket was decorated with red, white, and blue flowers. Tammy wishes Terry were still alive but is consoled, knowing that he could give Angilee a “hug for the first time in 38 years.”
Time And The Brain
To eulogize Terry and recall his remarkable life, emergence, and death, I want to consider the scientific legacy he left behind and what it implies for the future of disability rights for people with brain injury.
“Safeguarding the rights of people with disabilities is especially critical when their lives are marginalized by so many complicating factors.”
Over the past several decades, neuroscience has grappled with temporal questions about how long recovery from brain injury takes and how its pace varies. This question is linked with mechanisms of recovery and therapeutics and thus is central to neuroscientists’ framing of the underlying science. To that end, Terry’s narrative helped to rewrite expectations about time and the brain, revealing both biological processes of recovery and the contingent construction of knowledge in this field. Previously in these pages, I wrote about how a lack of temporal knowledge about COVID-19 complicated clinical practice and moral judgement during the early phases of the pandemic; a similarly shifting conundrum—the trajectory of brain injury—has plagued neuroscience for most of my career.
In 2003 the possibility of a late recovery from the vegetative state was unthinkable, indeed heretical. Terry’s awakening exposed the provisional nature of neuroscience’s knowledge about the trajectory of severe brain injuries and recovery—a conversation that began in 1972 when the vegetative state was first described by British neurosurgeon Bryan Jennett and American neurologist Fred Plum in a now-classic Lancet article. Half a century later, the article is as prescient for what it says as it is for what it doesn’t say when describing these brain states.
Jennett and Plum’s essay remains a study in interdisciplinary collaboration between two cross-Atlantic enantiomers whose talents came together to describe and name the vegetative state. Luminaries in mid-century neurology—Jennett developed the Glasgow Coma Scale, and Plum first described the locked-in state and was the court-appointed neurologist in the 1975 right-to-die case of Karen Ann Quinlan—each man held a piece of the puzzle to characterize the paradoxical clinical condition in which a patient can open her eyes, yet exhibits no apparent evidence of awareness of self, others, or the environment.
Jennett and Plum sought to make sense of this “syndrome without a name” by explaining the physiology and clinical characteristics of the isolated functioning of the brain stem without higher cortical functions. Although the name they chose has been interpreted by some to mean that individuals in that state were “vegetables,” the etymological and historical origins of the term “vegetative state” reveal the rich intellectual history of the way science understands consciousness.
“Terry’s awakening exposed the provisional nature of neuroscience’s knowledge about the trajectory of severe brain injuries and recovery.”
The use of the term vegetative originated with Aristotle’s De Anima (On the Soul), which distinguished plant-like functions from higher animalic ones. Borrowing from this typology, Jennett and Plum named the autonomic brain stem tasks that control breathing and heartbeat as vegetative in order to differentiate them from higher cortical ones that control thought and emotion. Their naming of the vegetative state is an elegant invocation of the history of science that contextualizes new discovery against an ancient text.
Equally noteworthy is how Jennett and Plum decided on the temporal description of the vegetative state. Reading the text 50 years after they wrote it, I can almost hear their debate. (I met Jennett late in his life and Plum was my teacher and later colleague at Weill Cornell Medical College.) Should the vegetative state be called persistent, permanent, or prolonged? After deciding on persistent vegetative state, they thought it critical to explain their reasoning and justify their choice, using the first person plural. “Certainly we are concerned to identify an irrecoverable state, although the criteria needed to establish that prediction reliably have still to be confirmed. Until then ‘persistent’ is safer than ‘permanent’ or ‘irreversible’; but prolonged is not strong enough, and unless it is quantified, it is meaningless.”
Jennett and Plum’s logic is what makes the essay so very prescient. Absent long-term epidemiological data about the time course of these brain states, they couldn’t be declarative in predicting when the vegetative state would become permanent. They knew what they didn’t know and so were cautious. By 1994, things had seemed to evolve. A New England Journal of Medicine multi-society task force report on the vegetative state concluded that a persistent vegetative state became permanent if it lasted three months after anoxic injury (inadequate oxygen getting to the brain in the setting of cardiac arrest or profound drops in blood pressure) and 12 months after a traumatic brain injury. That framework informed clinical thinking for over two decades, bringing with it notions of futility once “permanence” had set in.
“Their naming of the vegetative state is an elegant invocation of the history of science that contextualizes new discovery against an ancient text.”
That designation was reversed in 2018 when new data revealed that upward of 20% of those thought to be permanently vegetative—patients like Terry Wallis—could evolve into higher brain states. With this in mind, patients who remained in the vegetative state three months after anoxic injury and a year after traumatic injury were redesignated as being in the chronic vegetative state. The term chronic vindicated the foresight of Jennett and Plum in 1972 when they opted for “persistent” instead of “permanent” to designate the condition.
If the renaming of the permanent vegetative state as chronic is scientific confirmation of Jennett and Plum’s prudence, it is also part of Terry Wallis’s legacy. The protracted nature of his recovery defied temporal expectations about the return of consciousness long before experts thought this possible. If nothing else, it reminds would-be classifiers of illness to have nosological humility when working at the edge of knowledge.
Covert Consciousness
Questions of humility and uncertainty become even more salient in another part of Terry’s legacy—his narrative revealed the clinical paradox that what one sees at the bedside might be deceptive. What doctors observe in clinical practice may not reflect the true capacities hidden within an injured brain, which has important implications for the care of those with brain injuries who may be covertly conscious.
When I interviewed Terry’s mother, Angilee, a few years after he began speaking, she told me a story that suggested her son may have been aware as early as 1993. As I recounted in my book Rights Come to Mind, one morning she received a call from an aide at the nursing home where Terry lived, urging her to come to the facility to comfort her son. Angilee told me that the aide said Terry’s elderly roommate with advanced dementia had died overnight from suffocation after becoming entangled in his bedsheets. The aide thought that Terry seemed “bothered” and urged Angilee, “I [Angilee] needed to be down there.” The aide—who hadn’t been schooled in the characteristics of the vegetative state—didn’t know that doctors considered it technically impossible for a person in the vegetative state to respond to their environment or to be upset. As she told Angilee, both observation and her intuition told her that Terry needed his mother.
“What doctors observe in clinical practice may not reflect the true capacities hidden within an injured brain, which has important implications for the care of those with brain injuries who may be covertly conscious.”
Angilee explained that when she arrived, Terry wouldn’t go to sleep and he “was laying there with his eyes wide open.” She stayed there all day until he finally was able to sleep. Haunted by his response, especially in light of the fact that he had since recovered consciousness, Angilee worried that he might have been aware of his roommate dying or suffering. When I interviewed her years later, after Terry had begun to talk, she said, “So I don’t know what he saw, but I know he saw something. And … I knew then it had to be something that was really bad.” In the years after Terry recovered speech, Angilee’s feelings of unease that day had become even more terrifying to her. She had become convinced that his aberrant behavior after his roommate’s death indicated that he had been aware at some level.
I sensed that she wished she had better understood that Terry could have been in a liminal state of consciousness that night, so she might have been better able to console him. In retrospect, I wish I had consoled her when she told me about this. I would have wanted her to know that she did the best she could given what she knew at the time. Her experience is a vivid reminder that as science expands knowledge, it sometimes creates and exposes moral quandaries in its wake.
Although it is impossible to know precisely what Terry experienced that night, in the ensuing years functional magnetic resonance neuroimaging has demonstrated that patients who appear unconscious may in fact have a nonbehavioral response on brain scans. While in a scanner, a patient thought to be in the vegetative state was asked to follow a volitional prompt such as imagining playing tennis and navigating around the patient’s house. The prompts resulted in the activation of the motor cortex or parietal lobe—areas associated with these tasks—indicating that the patient was not unconscious but in a nonbehavioral, minimally conscious state. Schiff would later write of “cognitive motor dissociation” to describe the mismatch between brain activity and observable behaviors at the bedside.
“As science expands knowledge, it sometimes creates and exposes moral quandaries in its wake.”
Just as Terry’s story foretold the discovery of covert consciousness before neuroimaging confirmed it, Jennett and Plum’s literary precision also anticipated the possibility that what was seen at the bedside might tell only part of the story. In their initial description of the vegetative state, they observe, “It seems that there is wakefulness without awareness.” Here again, Jennett and Plum were prescient when they wrote that the vegetative state seems to be one of wakeful unresponsiveness. Based on the presence of a functioning brain stem and the absence of higher cortical function, on clinical examination they believed that the vegetative state was devoid of consciousness. But absent functional neuroimaging, which would only begin to probe the workings of the hidden brain in the 1990s, they could not know for sure. So they hedged and wrote that the vegetative state seems to be one of wakefulness without awareness. While Jennett and Plum did not explicitly suggest the possibility of covert consciousness, the logical implication of their cautionary wording suggests that it might have been possible. Their deep commitment to prudential wording—their nosological humility—reminds physicians and researchers today of the need to respect the limits of our knowledge and leave open the possibility that technological advance will provide additional insights in the future.
From Diagnosis To Therapy
In his 1894 essay entitled “The Leaven of Science,” renowned physician Sir William Osler said, “The determination of structure with a view to the discovery of function has been the foundation of progress.” Over the past two decades, neuroscience’s growing knowledge of the physiology of consciousness and mechanisms of recovery have underpinned the advance of nascent drug- and device-based therapies. The promise of these therapies, coupled with the rapid evolution of knowledge about consciousness, raises questions that society has barely begun to explore.
Central to today’s therapeutic approaches is the work done to elucidate the mesocircuit by Schiff, whose images in 2004 revealed hints of the physiology behind Terry’s brain recovery. The mesocircuit, demonstrated via studies of cerebral dysfunction in severe brain injury, highlights the key role that the central thalamus plays in linking the cortex, basal ganglia, and the brain stem in the support of consciousness. In this model, the thalamus functions much like an airline hub—analogous to the role Atlanta’s Hartsfield-Jackson Airport plays for Delta Airlines. All connections lead through Atlanta, and if there is a storm there, a traveler’s passage will be disrupted. The thalamus, similarly, acts as a way station for wide thalamo-cortical connections, which splay out into the cortex, with projections up from the brain stem arousal system. The former helps to integrate cortical function, and the latter provides arousal input necessary to sustain consciousness.
“The promise of these therapies, coupled with the rapid evolution of knowledge about consciousness, raises questions that society has barely begun to explore.”
Even an isolated thalamic injury can be devastating. Knowledge of the mesocircuit has informed a number of promising therapeutic approaches using deep brain stimulation (DBS) to activate dormant connections in the mesocircuit and restore the brain’s functional integration. In 2007, my colleagues and I reported on our experience using DBS in a 38-year-old man who had been in the minimally conscious state for six years following an assault. He initially had a low score for responsiveness, but he later evolved into the vegetative and then minimally conscious state with little more than an inconsistent ability to follow commands with eye movements. With stimulation, he recovered fluent language, improved limb control, and was able to eat by mouth for the first time since his injury. He was able to say six- or seven-word sentences, tell his mother he loved her, and voice a preference about clothing when she took him shopping at Old Navy. These improvements were directly associated with stimulation and constituted the first evidence that DBS could promote late recovery in severe traumatic brain injury.
Our research has continued with other people with moderate to severe brain injury, as reported in the New York Times. While much more needs to be done to turn this type of investigative work into established therapies, some trials have been encouraging and suggest the possibility of an emerging new intervention for a population currently looking for effective treatments.
A Right To Consciousness
When I started medical school, these vast questions around consciousness, treatment, time, rights, and responsibilities were not discussed or even considered. At the time, neuroscientists saw the vegetative state as one of futility, and so the dominant societal conversation was about the right to die.
The origins of the legal right to die in America was predicated upon the vegetative state that had been documented in the 1970s with Karen Ann Quinlan, and later with Nancy Cruzan and Terri Schiavo. Establishing this right for patients and families was vitally important, but the early association of the vegetative state with the establishment of the right to die has left an enduring presumption that severe brain injury is without hope. This historic legacy can lead to implicit bias and premature discussions about end-of-life care, even as neuroscientists have developed increasing hope for treating disorders of consciousness. Nearly a half-century after Quinlan’s death, Terry Wallis’s experience reflects these tragic, embedded assumptions.
Nonetheless, evolving knowledge has opened new clinical and normative horizons for brain injuries. With a better sense of the prevalence of covert consciousness, the temporal frame for brain recovery, and an expanding set of therapeutic possibilities, the widespread neglect of brain-injured patients has become a societal challenge demanding a comprehensive, humane approach. Learning to identify covert consciousness and predicting its course are projects for the future of the field. But now that these possibilities have been proven to exist, it is no longer acceptable to look away and presume the worst.
As the neuroscience about disorders of consciousness has evolved, it has become clear that society has a pressing ethical and legal obligation to view consciousness as a civil right: if it is present, it must be recognized; if insecure, it must be supported. As researchers develop the technological means to identify covert consciousness and then to restore and sustain people with disorders of consciousness, society must begin to see this as a responsibility concordant with disability law and the Americans with Disabilities Act (ADA).
“As the neuroscience about disorders of consciousness has evolved, it has become clear that society has a pressing ethical and legal obligation to view consciousness as a civil right.”
The ADA compels society to hear the voices of people with disabilities, respect their lives, and integrate them into the nexus of their families and communities. The law, and its aspirations, gives sobering context to the narrative of Terry’s life and death. And his death demonstrates that rights are necessary but not sufficient—they must be backed up by appropriate, accessible care, in every part of the country. Terry deserved better, and so do others who struggle under the burden of severe brain injury and are left isolated and away from the larger community.
Now that scientists are on the cusp of having the technological means to provide imaging, stimulation, and drugs that may allow for more human flourishing, the nation must begin to grapple more meaningfully with the care and regard of marginalized people with disorders of consciousness. Their plight is the civil right that we don’t often think about, but we must.
Joseph J. Fins is the E. William Davis Jr., MD, Professor of Medical Ethics and a professor of medicine at Weill Cornell Medical College. He is also a visiting professor of law and the Solomon Center Distinguished Scholar in Medicine, Bioethics, and the Law at Yale Law School. He is grateful to Tammy Baze and the Wallis family for their permission to tell their story.